Audit and awareness - how staff at Hexham General Hospital improved the delivery of time critical medication: best practice case study
Service improvement projects that focus on a specific issue and hospital ward can create positive impact.
This case study details how a dissertation led to an increase from 68.9% to 85% in the delivery of Parkinson's medication on time, on a ward at Hexham General Hospital.
- Care strategies
- Inpatient care and medicines management
- Service improvement
- Treatments and medication
- Case studies
- Q&As
- Doctor (Geriatrician)
- Doctor (Neurologist)
- Doctor (Other)
- Nurse (other)
- Nurse (Parkinson's nurse)
- Complex
- End of life
- Maintenance
We spoke to Katie Turnbull, a recently qualified staff nurse working at Hexham General Hospital, about the steps the team has taken and what they have learned from the project.
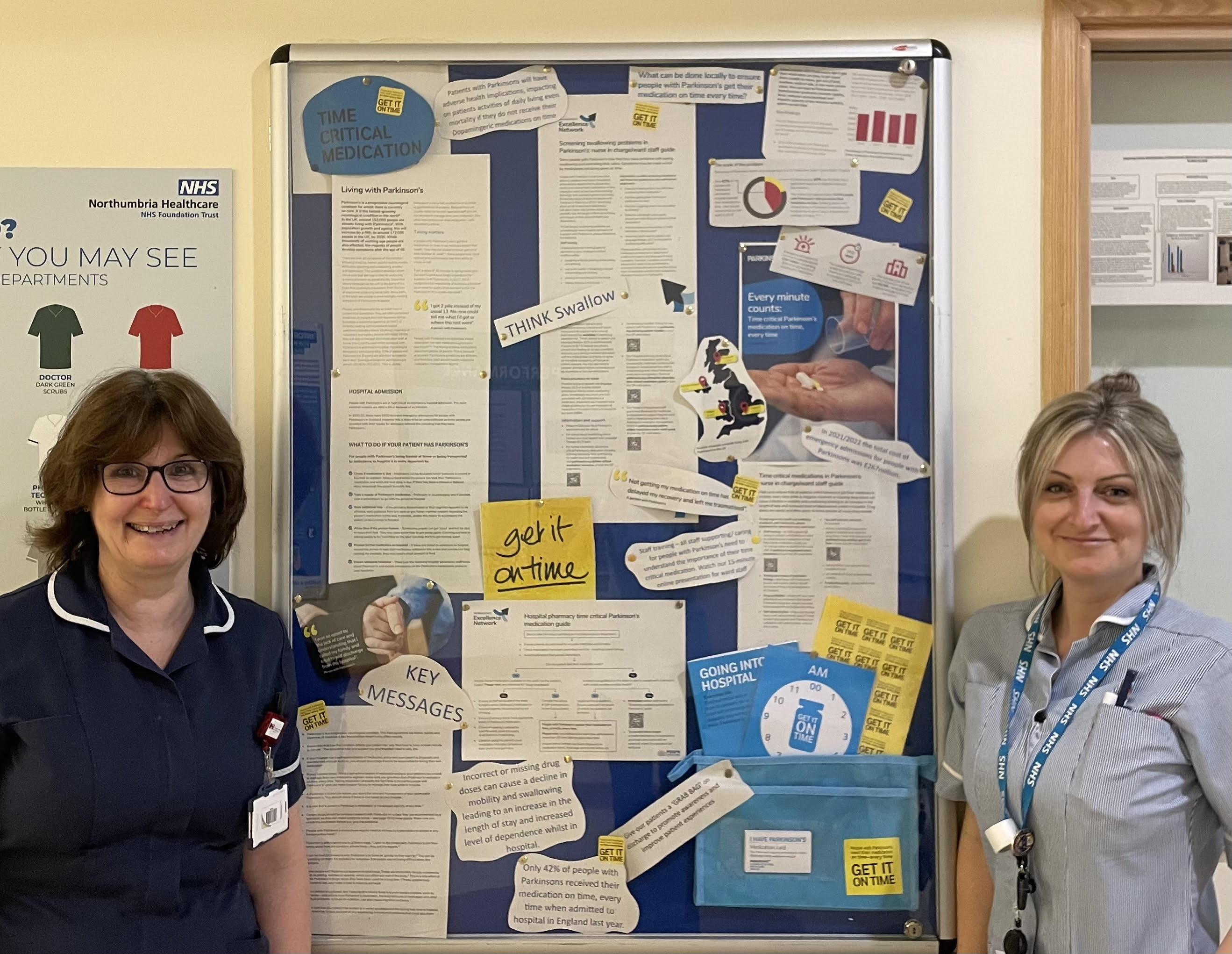
Left to right: Anne Bowman, Ward 2 Hexham General Hospital Manager; Katie Turnbull, Staff Nurse
Why did you work to improve the delivery of time critical Parkinson’s medication for your patients?
My dissertation was based on a service improvement initiative designed to improve the delivery of Parkinson's medication on time, every time.
While I was working on my dissertation, I recognised that patients with Parkinson's receive sub optimal care while they're in hospital, an area that the National Institute of Health and Care Excellence (NICE) admits is underdeveloped. I found that patients didn't always receive their Parkinson's medication on time, and only 60% of consultants said they were confident that their patients received their medication on time.
Medication delays can cause a huge amount of unnecessary distress and anxiety for both patients and their family members. Further research highlighted there is a strong link between lack of staff education and lack of readily available medication.
Administration of Parkinson's medication on time is essential for effective management of the condition. If patients with Parkinson’s don't receive medication on time, it can have adverse health implications, impacting patient’s activities of daily living, and even leading to death.
There is evidence to suggest that patients with Parkinson’s may not make a full recovery after discharge. This is an alarming discovery when patients are in the care of healthcare professionals who are regarded as experts.
Finally, my research identified a significant correlation between delayed, missed or omitted medication and prolonged hospital admissions and increased NHS costs.
What have you done to improve the delivery of time critical Parkinson’s medication?
I introduced an awareness campaign, using a display board at the entrance to our ward for staff, patients and visitors. I hoped this would provide a learning opportunity for staff to reduce medication errors in people with Parkinson’s.
Weekly staff meetings gave me the opportunity to raise awareness, highlight concerns and update colleagues on new strategies. I also distributed information, including the Excellence Network's "Caring for your patients with Parkinson's" booklet.
Alongside this, we initiated the use of visual prompts, such as the laminated clocks that nursing staff can mark dose times on. Using the free Parkinson’s UK resources, I provided ‘grab bags’ which we gave to people with Parkinson’s when they were discharged. This included the "Going into hospital" booklet, a medication card, Get It On Time stickers and laminated clock, to help them feel better prepared for any future admissions.
We encouraged patients to keep spare Parkinson's medication inside the bags and asked them to bring these with them if admitted to hospital or coming to an appointment. The bag would be a visual prompt for healthcare professionals to help them identify people with Parkinson’s early and avoid missing Parkinson's doses.
The study took place over 6 months from August 2023 to February 2024. I extracted data from our electronic prescribing system (Triscribe) to explore the number of doses scheduled and compared this to the time the dose was administered: on time, early, late or omitted. This established if the service improvement intervention had made a difference and if it had improved the delivery of Parkinson's medication on time.
Tips for hospitals: how to improve the delivery of time critical medication
- Data collection and analysis: start by collecting data on current medication administration practices, including timing, adherence rates, and any challenges encountered. Analyse this data to identify areas for improvement.
- Multi-disciplinary team collaboration: involve colleagues from a variety of departments, including neurology, pharmacy, nursing, and administration, to gain diverse perspectives and expertise.
- Education and training: provide comprehensive education and training sessions for staff members involved in medication administration. Make sure they understand the importance of timely administration and have the knowledge and skills to execute it effectively.
- Patient awareness: inform patients and their caregivers about the importance of sticking to medication schedules and the potential consequences of missed doses. Provide resources and support to help them manage their medications effectively.
- Continuous monitoring and improvement: regularly review processes and adjust as needed to optimise efficiency and effectiveness using the plan, do, study, act (PDSA) cycle.
What impact has this project had on patients?
Data collection started 121 days before the intervention to establish a baseline. Due to time constraints, data was collected for only 88 days after the intervention.
The data shows that after the intervention, we increased the timeliness of Parkinson's medication from 68.9% to 85%.
Patients and their families have recognised the ‘grab bags’ as a useful tool and educational resource for families.
I have received positive feedback from colleagues about the use of the visual aids and this is now a well established practice on the ward.
Did you involve people with Parkinson's in the project?
My dissertation initially began with a literature review, but during the implementation phase, I involved patients with Parkinson's, their family members and carers in the process. These experts with lived experience can provide invaluable insights into what it is like living with Parkinson's, and their input was very beneficial.
I involved patients in the decision making processes, keeping them informed about the service improvement progress, and actively seeking their input at all key stages.
This sounds like a real team effort, which teams have been involved in this project?
My manager Anne Bowman has supported my project, and this topic has become one of the ward's objectives. Nursing staff helped initiate the project and continue to implement it when I have not been on duty. Without their support, this project wouldn't have been successful.
I also sought advice from our pharmacy team, and a pharmacy technician who is the team leader for informatics supported me with the Triscribe software.
Medication errors and timeliness of Parkinson's medication has been one of the trust's main quality priorities since 2023, and will continue through 2025. This work has aligned with the wider focus on this issue across the trust. For example, a separate project is taking place at the Northumbria Specialist Emergency Care Hospital in Cramlington which also aims to improve the timeliness of Parkinson's medication.
How have your colleagues across the hospital worked collaboratively on this project?
Collaboration across departments was crucial for the project to succeed. My colleagues have contributed by:
- providing data on current medication administration practices
- sharing insights on patients' needs
- offering suggestions for improvement
- participating in training sessions to ensure consistent implementation of best practice.
Overall, this project wouldn't have been as successful without that buy-in from colleagues across the hospital.
Related resources
Explore the resources and materials that have supported this service improvement project, and related best practice case studies:
- Time critical medication and Get It On Time campaign resources
- Order time critical medication promotional materials
- Caring for your patient with Parkinson's: booklet
- Benchmarking to improve the delivery of time critical medication at South Tyneside and Sunderland NHS Foundation Trust
- Self administration: a patient-centred approach to administering time critical Parkinson’s medication at University Hospitals of Leicester NHS Trust
- Improving the delivery of time critical medications at Bradford Teaching Hospitals NHS Foundation Trust

